Non-epileptic Paroxysmal Episodes In Children
Paroxysmal nonepileptic episodes (PNED) are a group of recurrent , sudden-onset, short-term disorders that frequently appear in children. They are disorders much more frequent than epilepsy, although they are not as popularly known. Its prevalence is between 5 and 20% in the child population. Approximately 10 out of 100 children and adolescents suffer from some POST in their lifetime.
It is important to know what they are in order to differentiate them from other disorders, such as seizures or febrile seizures. If they are diagnosed early, their cause can be found and unnecessary treatment avoided. Learn more about them in this article.
How are paroxysmal episodes classified?
Paroxysmal episodes can be epileptic and non-epileptic. However, today we will focus solely on the latter in order to study them in more detail.
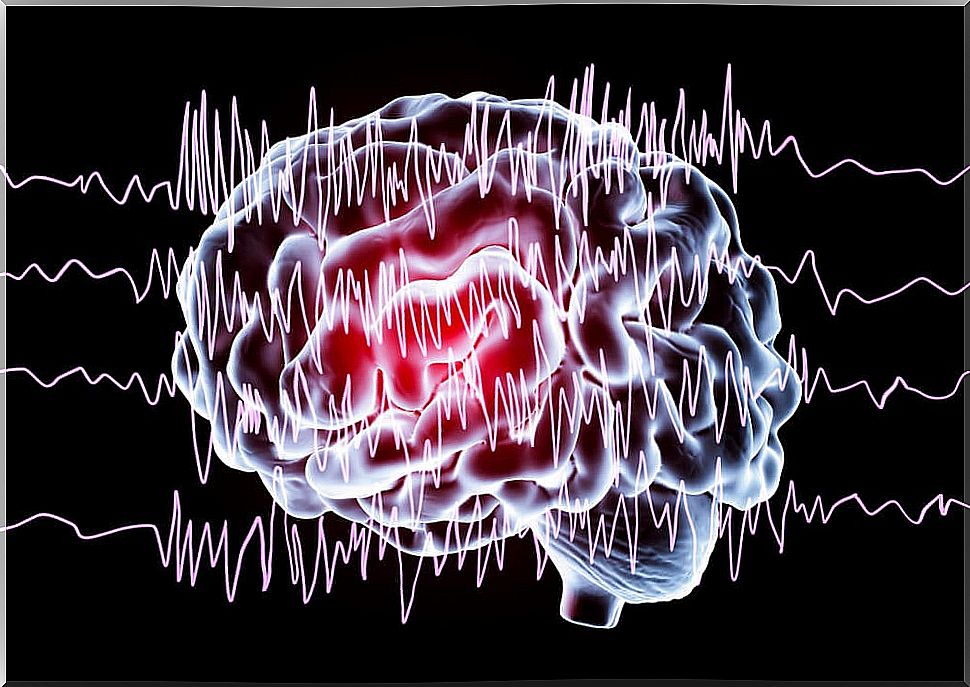
As we have said, NEPTs include a set of diverse disorders produced by dysfunctions in the brain, with the particularity that they are not caused by neuronal hyperactivity, as occurs with epileptic disorders.
They can be classified into several groups according to their clinical manifestations:
- Brain hypoxia. They are the most frequent TPNE. They are caused by a temporary loss of consciousness due to a reduction in cerebral blood flow.
- Neonatal apnea.
- Spasms of sobbing.
- Syncopes.

- Paroxysmal sleep disorders. They are the ones with a more benign character, generally.
- Narcolepsy or cataplexy.
- Somnambulism.
- Obstructive Sleep Apnea Syndrome (OSAS).
- Night Terrors.
- Nightmares.
- Rhythmic movements in the transition from sleep to wakefulness.
- TPNE engines. They are characterized by involuntary and jerky movements.
- Benign myoclonus of the infant.
- Benign paroxysmal torticollis of the infant.
- Infant paroxysmal benign ocular deviation.
- Sandifer syndrome.
- Spasms nutans .
- Tics.
- Shudders.
- Hyperekplexia.
- Iatrogenic dyskinesias.
- Newborn tremulations.
- Stereotypies and motor rhythms.
- Secondary to systemic diseases.
- Respiratory.
- Cardiac.
- Digestive
- Metabolic
- By drugs or drugs.
- Psychological or psychiatric. They occur especially during adolescence and are becoming more frequent.
- Tantrums
- Panic and anxiety crisis.
- Hyperventilation
- Pseudo-crisis.
- Self-stimulations.
- Münchausen syndrome by proxy.
- Others.
- Migraines.
- Benign paroxysmal vertigo.
- Myoclonus of the soft palate.
As we can see, the TPNE are many and very diverse. Often, we have heard of some of them separately, but we must know that they fit within this group in order to better understand their causes. In general, all have a benign character.
Diagnosis
Diagnosis is a very important point in POSTs since, as we have said, we can avoid many unnecessary antiepileptic treatments and many family anxieties that often arise as a result of the diagnosis of epilepsy.

To make a good diagnosis of these disorders, it is necessary to study the medical history in detail and carefully observe the paroxysmal events. Sometimes some symptoms complicate the differential diagnosis. These are, for example:
- The alteration of the level of consciousness.
- The abnormal movements.
- The abrupt and sudden appearance, without warning.
Many times, the errors of diagnosis are due to the ignorance of these disorders, or to the overestimation of a family history of epilepsy or a history of febrile seizures, for example.
A physical and neurological examination will also help rule out other conditions. Sometimes, it is necessary to resort to complementary tests, such as the electroencephalogram (EEG). Other tests that can help are, for example:
- Cardiology studies.
- Psychiatric studies.
- Neuroimaging tests.
- Sleep studies.
- Hormonal studies.
Treatment
After a correct diagnosis, the treatment will depend on the specific PNET and the cause of its appearance. In most cases, no treatment is necessary.
In general, it is enough to know what we are facing in order to rule out epilepsy, remove fear and normalize situations.